Table of Contents
This page will teach you about heart disease and how it can be prevented and treated with a healthy lifestyle.
Section 1: What are Coronary Artery Disease (CAD) and Hyperlipidemia?
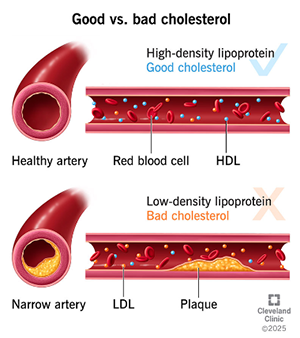
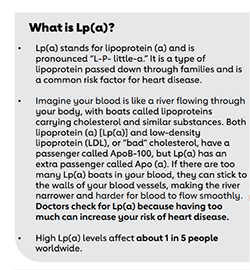
Coronary artery disease (CAD) is a condition in which the blood vessels that supply the heart with oxygen and nutrients become narrowed or blocked due to a buildup of plaque in the artery wall known as atherosclerosis. Plaque deposition is often preceded by damage to the inner layer of the arteries which is the endothelium. This endothelium can become damaged from multiple factors including smoking, diabetes, high blood pressure, obesity, and high cholesterol that all increase inflammation and oxidative stress. Once the inner endothelium has been damaged this makes it easier for plaque deposition to take place. Plaques are primarily composed of cholesterol and fat that form as a consequence of elevated LDL “bad” cholesterol circulating in the blood.
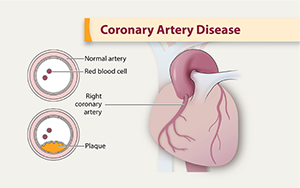
Over time, plaque can accumulate inside arteries, similar to how residue builds up in a car’s fuel line. This buildup causes narrowing that restricts the amount of blood that can reach the heart, much like a partially clogged fuel line limits the flow of fuel.
For further information about CAD, the following resources would be quite beneficial:
Section 2: Why Should I Care?
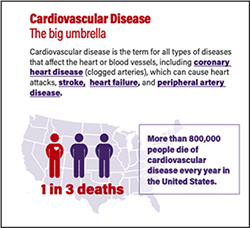
Cardiovascular disease includes a group of conditions that affect the heart, with the most common condition being CAD. This group of diseases is the leading cause of death in the United States and affects approximately 20.5 million adults.
Traditional risk factors for CAD include high LDL “bad” cholesterol, low HDL “good” cholesterol, high blood pressure (hypertension), family history, diabetes, smoking, and obesity. Additionally, the risk of CAD increases after age 45 in men and after age 55 in women. For people with risk factors and even those without clear risk factors it is important that we take steps to lower risk.
Section 3: How are CAD and Hyperlipidemia harmful to my body?
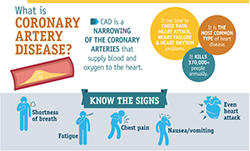
When cholesterol plaques cause narrowing of the vessels that supply the heart, it doesn't receive enough blood and is starved of oxygen. This can lead to chest pain (angina), especially during physical activity or stress. If a plaque breaks open, it can form a blood clot that completely blocks the artery, akin to a completely clogged fuel line, resulting in a heart attack. The same process can occur in other arteries in your body. If it occurs in the carotid arteries of your neck it can lead to a stroke. If it occurs in the legs it can cause pain with walking also known as claudication.
Symptoms of CAD vary but commonly include chest pain (angina), upper back or neck pain, heartburn, shortness of breath, nausea or vomiting, fatigue, and heart racing which may initially manifest during physical exertion or strong emotional responses. Without treatment, CAD progresses, leading to more frequent and severe symptoms and potentially a heart attack.
Sources:
Section 4: How Do I Know if I have CAD or Hyperlipidemia?
Hyperlipidemia is diagnosed by measuring various cholesterol levels such as low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides (TG) on a blood test called a lipid panel.
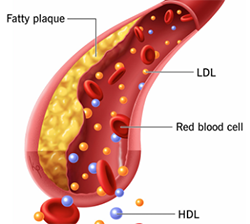
Other blood tests such as an Apolipoprotein B (ApoB) and Lipoprotein A (Lpa) may also be ordered by your doctor to further assess your risk.
CAD can be diagnosed by tests such as a cardiac CT, coronary calcium scan, stress test, and invasive catheterization that looks directly at the arteries.
For further information about lipid panel indices, ApoB, Lpa and more, consider the following podcasts:
- What Causes Cardiovascular Disease with Dr. Dayspring
- Assessing Your Risk of Cardiovascular Disease with Dr. Dayspring
Section 5: How can CAD and Hyperlipidemia be treated?
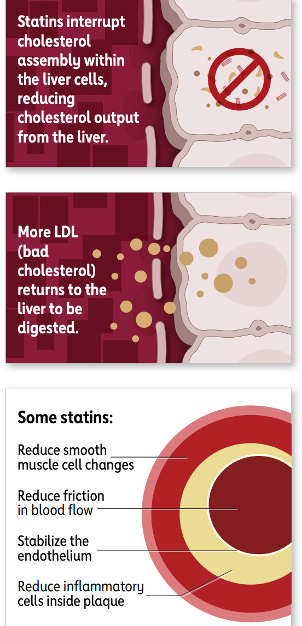
As previously discussed, CAD and hyperlipidemia can develop as a result of elevated levels of “bad” cholesterol in the bloodstream. These cholesterols are strongly influenced by our diet and lifestyle, so leading a healthy lifestyle is imperative in treating these conditions. In addition, there are also medications that your doctor may prescribe, such as statins, ezetemibe (zetia), PCSK9 inhibitors (repatha), and more.
The most commonly prescribed cholesterol-lowering medications are statins. These medications work in the liver to prevent the production of cholesterol which lowers the circulating levels in the blood. Examples of statins include: atorvastatin, rosuvastatin, pravastatin, simvastatin.
For detailed information about cholesterol-lowering medications, LISTEN to the following PODCASTS:
Section 6: How Can a Healthy Lifestyle Prevent and Treat CAD and Hyperlipidemia?
Diet:
High cholesterol levels in the blood induce inflammation and oxidative stress that damages the blood vessel walls and leads to plaque formation and the blockages that can cause a heart attack. These plaques are largely composed of cholesterol and fats, so modifying the diet to reduce saturated and trans fats while increasing unsaturated fats like polyunsaturated and omega-3 fatty acids is essential to treat and prevent this process.
Dietary saturated fat intake is the main driver of increased LDL cholesterol and Apolipoprotein B. A heart-healthy diet, reduces or eliminates saturated fats and promotes plant-based food to prevent and manage CAD and hyperlipidemia. While a whole food plant-predominant diet can lower LDL cholesterol and apolipoprotein B levels effectively, it also decreases the risk and severity of other chronic diseases like diabetes, hypertension, dementia and cancer.Many patients also find that this same diet improves their energy levels and sleep, allows them to lose weight, and live healthier active lifestyles.
There are many types of dietary fats in the typical American diet, but the fats that play the biggest role in directly forming plaques are saturated and trans fats. Saturated fats are named because of their chemical structure and are unique in that they are most often solid at room temperature. Foods with very high levels of saturated fats include butter, palm and coconut oil, cheese, and red meat.
In the typical western diet, the largest sources of saturated fat intake are from:
- #1 Meat: Beef, pork and lamb contain the most saturated fat, but Americans get the most saturated fat from chicken and turkey because they eat so much of it.
- #2 Dairy: Notably full-fat dairy products such as cheese.
- #3 Ultra-Processed foods: These include cookies, cakes, crackers that contain significant additives and saturated fats such as butter
Vegan processed foods are also high in saturated fats due to palm and coconut oil and should be avoided.
In addition to reducing saturated fat sources in the diet, it is also important that we optimize the diet by maximizing the intake of foods that can further decrease saturated fat and cholesterol to improve endothelial health and reduce inflammation.
Robust evidence shows that the dietary pattern most effective in lowering LDL and apolipoprotein B is the Portfolio diet, which is rich in vegetables, plant-protein, nuts, seeds, whole grain fiber, and monounsaturated fats such as extra-virgin olive oil. This eating pattern lowers LDL levels (bad cholesterol), improves endothelial function, and reduces the risk of cardiac events. The Portfolio diet has specifically been shown to lower LDL cholesterol by 17%, Apolipoprotein B by 15%, and inflammatory marker CRP levels by 32% with one study showing that this diet confers a LDL-lowering effect similar to lovastatin 20mg.
In addition to the Portfolio Diet, there are also other eating patterns that have shown strong evidence for lowering LDL cholesterol and the risk of heart disease, most notably the Mediterranean diet. In comparison to the portfolio diet, this diet also emphasizes fruits and fish. When compared to a low-fat diet, the Mediterranean diet is associated with a significant reduction in the progression of plaque formation and cardiovascular disease risk. The Lyon Heart Study and Predimed studies have both reinforced strong evidence of cardiovascular disease protection with this eating pattern.
The Mediterranean diet, which is rich in fruits, vegetables, whole grains, nuts, and olive oil, reduces CAD progression and cardiovascular events. It is important to note that this diet along with the Portfolio diet includes certain cooking oils such as olive oil. But are all cooking oils created equal? The short answer is no! The best cooking oils are those that include a high composition of monounsaturated fats and a low composition of saturated fats, which contribute to elevated LDL and plaque formation.
The healthiest oils to cook with include:
- #1: Olive oil
- #2: Canola oil
- #3: Avocado oil
Plant-based diets are linked to lower CAD risk, and both the American College of Cardiology and the American Heart Association recommend these diets for cardiovascular health. Focusing on specific nutrients like omega-3 fatty acids, soluble fiber, and plant sterols can improve lipid profiles, with fish oil significantly lowering triglycerides. The DASH diet, emphasizing fruits, vegetables, and low-fat dairy, reduces blood pressure and long-term cardiovascular risk. Overall, adopting a diet rich in unsaturated fats, whole grains, fruits, vegetables, and nuts while reducing saturated and trans fats leads to significant improvements in lipid profiles, blood vessel function, and overall heart health.
In addition to lowering saturated fat and cholesterol, how do the Portfolio and Mediterranean diets reduce heart disease risk?
The endothelium, the lining of your arteries, is metabolically active and plays an important role in preventing atherosclerosis and heart disease. When the endothelium functions properly, plaque does not build up in the artery wall and existing plaque can actually start to recede. Nitric oxide is a vital molecule that is produced in healthy endothelial cells. It acts to dilate and relax the artery wall and promotes normal blood pressure.
Eating foods high in nitric oxide precursors helps to support artery health. Daily consumption of leafy greens, especially arugula (video on nitrate-rich vegetables), and non-green vegetables like beets (video on foods that protect arteries) can increase nitric oxide levels to promote endothelial health. Additionally, limiting sodium (salt) while increasing potassium through foods such as bananas helps promote nitric oxide release (video on sodium and arterial function).
Interested in learning about other ways a healthy lifestyle can promote a healthy endothelium? See below for additional resources.
- Lifestyle factors that boost endothelial cells - Quit Smoking, increase aerobic exercise like walking, avoid saturated fat and consume more berries, onions and green tea.
- Sleep deprivation causes endothelial dysfunction - Study shows sleeping less than 7 hours a night causes significant endothelial dysfunction
For further information about diet and CAD, the following resources would be quite beneficial:
- Prevent and Reverse Heart Disease by Dr. Caldwell Esselstyn
- Optimal Diets for Prevention of Coronary Heart Disease.
- Mediterranean Diet Reduces Atherosclerosis Progression in Coronary Heart Disease.
- Guideline on the Primary Prevention of Cardiovascular Disease.
- Diet, Exercise and Weight Loss and Dyslipidaemia.
- Effects of Diet on 10-Year Atherosclerotic Cardiovascular Disease Risk.
Physical Activity:
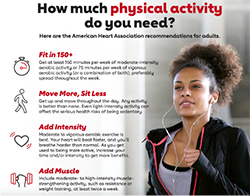
The American Heart Association (AHA) highlights physical activity as essential in preventing and treating atherosclerotic cardiovascular disease. Robust evidence has consistently shown that physical activity is linked to a lower incidence of CAD and plaque regression through enhancing endothelial function, increasing nitric oxide production, and reducing inflammation.
Given the robust data supporting exercise for prevention and treatment of CAD, the American College of Cardiology in collaboration with the AHA recommends that patients with CAD without contraindications to exercise should perform moderate-intensity aerobic exercise at least 150 minutes per week or at least 75 minutes of high-intensity aerobic exercise. Aerobic exercise includes activities such as brisk walking, cycling, or swimming. In addition, resistance (strength) training exercises are also recommended at least 2 days per week to improve muscle strength and for cardiovascular risk factor control.
Long-term exercise, especially when paired with a plant-based diet slows artery narrowing and improves blood flow to the heart. Moderate and high intensity exercise including walking, cycling, or swimming can be powerful for heart health when practiced consistently.
For further information about physical activity and CAD, the following resources would be quite beneficial:
- Physical Exercise and Its Effects on Coronary Artery Disease.
- Exercise and Inflammation in Coronary Artery Disease.
- Differential Effects of Aerobic Exercise, Resistance training, and Combined Exercise Modalities
Sleep
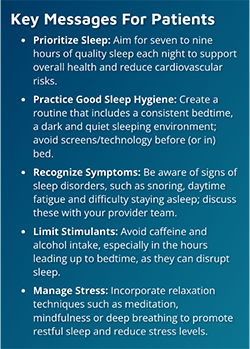
Sleep quality and duration play critical roles in influencing incidence and progression of CAD. Studies show that sleeping less than seven hours per night leads to significant endothelial dysfunction and is associated with an increased risk of developing CAD and cardiac events.
Poor sleep quality is also associated with worsening CAD, with a study showing that poor scores on the Pittsburgh Sleep Quality Index (a self-questionnaire assessing sleep quality) was linked to disease progression. Additionally, irregular sleep patterns are associated with CAD. The Multi-Ethnic Study of Atherosclerosis found that inconsistent sleep duration increased coronary artery calcium, indicating higher CAD risk. Both short and long sleep durations raise CAD risk, with the lowest risk at 7-8 hours of sleep per night. One study shows that each hour, less than or more than seven hours, increased CAD risk by 11% and 7%, respectively.
For further information about sleep and CAD, the following resources would be quite beneficial:
- Sleep Duration and Myocardial Infarction.
- Sleep Quality, Sleep Duration, and the Risk of Coronary Heart Disease.
- Nocturnal Intermittent Hypoxia and Short Sleep Duration Are Independently Associated With Elevated C-reactive Protein Levels in Patients With Coronary Artery Disease.
- Sleep Irregularity and Subclinical Markers of Cardiovascular Disease.
Stress:
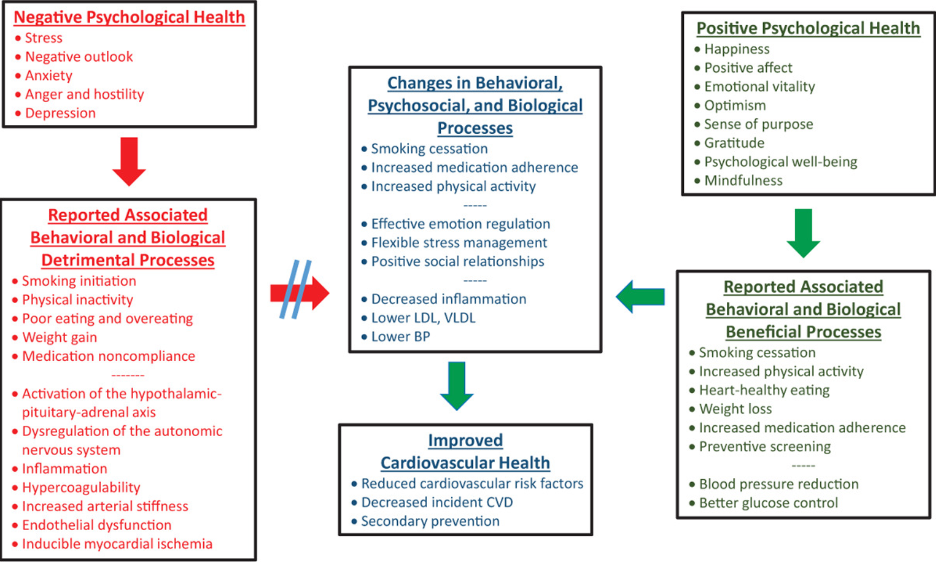
Emotional and physical stress sets off a hormonal cascade releasing adrenaline and cortisol which increases the heart rate and liberates glucose into the blood. In the short term this has many adaptive benefits, but when humans experience chronic stress this can lead to deleterious consequences.
Chronic stress significantly increases coronary artery disease (CAD), influencing both its development and progression. Increased levels of stress hormones can trigger heart attacks and irregular heart rhythms by increasing the heart rate and blood pressure. Chronic stress speeds up atherosclerosis, a key cause of CAD, by damaging blood vessels and increasing inflammation.
Chronic stress can cause mental health disturbances such as depression, anxiety, and social isolation that can also lead to unhealthy habits like poor diet and smoking, further raising CAD risk. The American Heart Association stresses the importance of managing these psychosocial factors in treating CAD. In summary, chronic stress significantly impacts CAD, highlighting the need for effective stress management for heart health.
Sources:
- Mental Stress and Cardiovascular Health.
- Chronic Stress: A Critical Risk Factor for Atherosclerosis.
- Stress and Atherosclerotic Cardiovascular Disease.
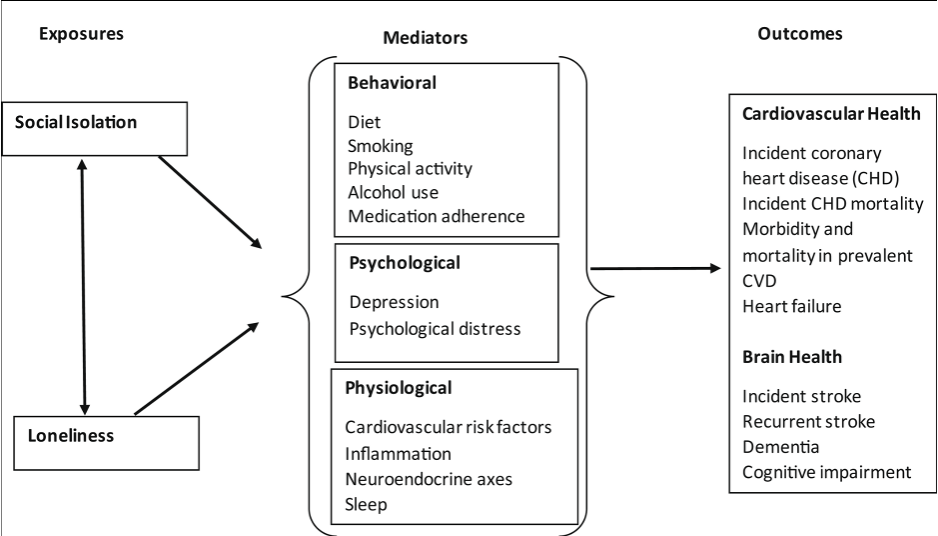
Social Connectedness
Positive social relationships are linked to improved heart health and a lower risk of CAD. For example, one study showed that women with high levels of emotional support have slower artery narrowing. Proposed mechanisms for these findings are through reductions in stress hormones, lower inflammation, and avoidance of cardiovascular risk factors.
In contrast, social isolation and loneliness increase the risk of CAD and lead to worse outcomes. Isolation is associated with higher levels of C-reactive protein, a marker of inflammation, which raises the chances of CAD mortality. Poor social relationships increase cardiovascular disease risk by 16%, and isolation predicts higher cardiovascular disease incidence and mortality, especially in older adults. The American Heart Association highlights the negative effects of isolation on heart health and the need for interventions. In summary, healthy relationships are associated with protection against CAD, while isolation and loneliness increase risk and worsens outcomes.
Sources:
- Intimate Relationships, Individual Adjustment, and Coronary Heart Disease: Implications of Overlapping Associations in Psychosocial Risk.
- Influence of Social Support on Progression of Coronary Artery Disease in Women.
- Social Isolation, C-reactive Protein, and Coronary Heart Disease Mortality Among Community-Dwelling Adults.
- The Impact of Social Isolation and Loneliness on Cardiovascular Disease Risk Factors.
- Effects of Objective and Perceived Social Isolation on Cardiovascular and Brain Health.
Harmful Substances
Cigarette Smoking
Smoking is a major risk factor for CAD. It induces oxidative stress, which decreases the production of beneficial nitric oxide in endothelial cells and increases harmful molecules like superoxide anion and malondialdehyde (MDA). This leads to poor blood vessel function, reduced ability of blood vessels to relax, and increased inflammation. Smoking also induces a pro-thrombotic state by increasing platelet stickiness and activating clotting factors.
Alcohol
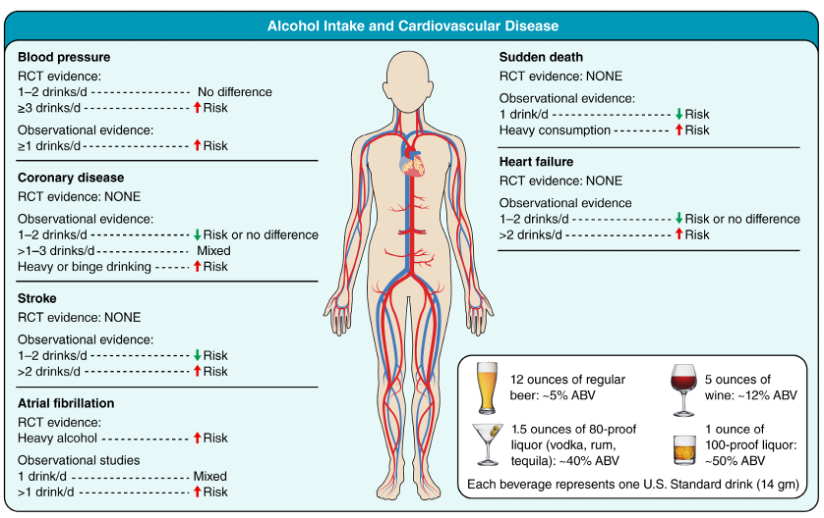
The relationship between alcohol intake and cardiovascular health has a complicated and controversial history. For decades moderate alcohol intake was thought to be neutral if not beneficial for cardiovascular health, but recent evidence raises robust evidence to support the contrary. Prior observational studies illustrated a J or U-shaped association between alcohol and CAD with modest intake (1 drink/day for women and 1-2 drinks/day for men) linked to lower CAD risk compared to abstinence. However more recent genetic and epidemiological evidence has indicated that even modest alcohol intake may indeed increase CAD risk and that this apparent protective effect seen in prior studies may have been due to confounding by healthier lifestyle factors among moderate drinkers.
Evidence suggests that increased alcohol intake accelerates CAD by inducing dyslipidemia, inflammation, and insulin resistance. The American Heart Association recommends reducing alcohol intake to ≤2 drinks/day for men and ≤1 drink/day for women may provide some risk reduction for CAD while excess drinking strongly increases risk for CAD.
Drugs
Illicit drugs such as cocaine and methamphetamines have several deleterious effects on the heart and blood vessels. Cocaine causes the release of stress hormones that increase the heart rate, blood pressure, and cardiac oxygen needs that can lead to acute cardiac events. Methamphetamine use is linked to oxidative stress, poor blood vessel function, and faster plaque buildup, significantly increasing the risk of heart attack.
In summary, substances like cigarettes, alcohol, and illegal drugs worsen CAD by causing oxidative stress and damaging blood vessels.
Additional Resources: